Advancements in surgical technology and therapeutics have improved outcomes for many cancer patients, resulting in 18 million survivors (and growing). New and more efficacious cancer drugs are being approved monthly. Radiation therapy can be targeted to decrease the toxicity and reduce the time of treatment by nearly 50%. And in some cases, surgeons can use robotic systems to resect the hardest-to-reach tumors. So, surely cancer care is getting better…right?
Yes, but… these achievements are still coupled with a poor patient experience, a capacity-constrained workforce, and unsustainable costs.
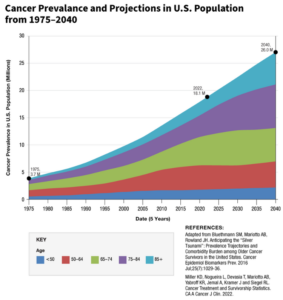
The cancer care journey is fraught with fragmentation and complexity, manifesting in significant challenges for patients in accessing and navigating care. Unfortunately, the number of patients who must endure this journey continues to grow, with both the aging of the population and concerning increase in diagnoses among young adults. This rise in incidence has severe implications for an already constrained oncology workforce that faces impending and critical shortages. Compound these problems with soaring cancer costs, which have resulted in a heightened focus from both public and private players pursuing oncology centric value-based care models to curb spend.
How do we get ahead to prevent the gut wrenching, life altering diagnosis? How do we extend the workforce and navigate patients to the right settings of care during their treatment journey? And what do all these advancements mean for the growing number of survivors? The answers to these questions have been answered, at length, from several viewpoints. However, I argue that innovative models focused on cancer care must put the emphasis on complete and thorough solutions to get at the real pain points that exist across the care continuum.
Early Detection or Diagnosis: An Opportunity to Diversify the Definition of “Good Outcomes”
Cancer outcomes have been shown to improve when the disease is detected at its earlier stages. We can sometimes simplify early detection by 1) identifying patients at risk and 2) getting them screened. Yet the chasm between those two steps is significant.
Many early detection platforms tout their analytical and technical capabilities to better stratify patients, thereby solving the first challenge. However, what becomes more critical is surfacing this information at the appropriate time, motivating patients to actually get screened, mitigating barriers, and facilitating next steps based on the screening in partnership with the patient’s integrated care team.
Barriers to screening exist, especially for disadvantaged individuals from lower socioeconomic backgrounds, as well as those from underrepresented ethnic groups, and individuals who are uninsured or underinsured. Moreover, these disparities in cancer screenings only exacerbate the disparities in cancer outcomes. Identifying patients is half of the battle but getting them screened and tied back into their provider is the persistent pain point. Addressing access challenges and understanding motivations will lay the groundwork for processes and systems that bridge that gap.
By nailing the continuum of early detection, we can diversify the definition of good outcomes in cancer care beyond survivorship. As a result, our care delivery system could then also start to laud improved prevention outcomes and a growing number of “pre-vivors”.
The In Between and Active Treatment: Why Innovation Must Focus on Patients and Providers
Amidst the distress caused by a cancer diagnosis, patients are left to sort through vast amounts of information, treatment options, and concerns around efficacy and side effects, while juggling other life activities. Delays in treatment are common due to patient inertia or fear, or capacity constraints among providers. Moreover, the vast and growing knowledge in the field motivates many oncologists to sub-specialize. While sub-specialization can improve the quality of care, it can also exacerbate workforce shortages and barriers to patient access. In this rapidly evolving cancer care paradigm, it has become increasingly important to support both patients and providers.
The Centers for Medicare and Medicaid Services (CMS) recently approved reimbursement for patient navigation services that apply to patients with cancer. This provides a payment structure for a navigator to help patients with managing referrals, appointments, and social support programs. Although this represents a notable tailwind, the needs of patients extend beyond logistics. Holistic care management should not only support patients while on treatment, but also with their treatment. This includes new needs that arise around symptom management, medication management, and behavioral health. In my research on the oncology landscape, I spoke with Dan Nardi, CEO at Reimagine Care, who emphasized the impact of comprehensive wraparound services. Not only do these services improve the patient experience but they also enhance clinical outcomes.
On the provider side, clinical decision support technology can help inform treatment plans and recommendations by integrating vast amounts of data and guidelines, utilizing AI capabilities, and surfacing insights. These solutions can even facilitate shared decision-making, distilling the information and making it more digestible for the patient to remain informed. While these solutions show immense potential, beware of the fixation on the flashy technology at the expense of neglecting the fundamental challenge of gathering and consolidating the data that exists across disparate sources. Some providers are already hesitant to embrace decision support tools. They become less incentivized when the integrity and completeness of the foundational data cannot even be trusted.
For example, I’ve spoken with Dr. Stephen Schleicher, medical oncologist and former chief medical officer at Tennessee Oncology, who reinforced the importance of developing a value-add tool that clinicians actually want to use. He believes little value will be added for clinicians until the entire picture is complete based on mutational data, clinical characteristics, and the nuances of the actual patient in front of them.
Finally, the debate on technology or AI displacing doctors has become trite and lands at the same conclusion: It won’t. Part of the role of the oncologist is still to understand the data and make the treatment recommendation. These tools do not diminish the clinical craft or expertise of providers, but should ease their day-to-day workflows.
Beyond Treatment: Empowering Survivors with Purpose-Built Models and Supportive Tools
As patients move beyond active treatment, clinical models need to adapt to their needs and preferences. This includes the needs of the growing number of survivors.
Previously, cancer survivors could expect, at best, a care plan and information packet. More comprehensive care platforms now exist to provide services for survivors who are dealing with complex physiological and behavioral health needs post-treatment, while often struggling to establish care with providers reticent to treat survivors. From lingering side effects to post-treatment surveillance and anxiety around recurrence, survivors need purpose-built models and supportive tools.
Through my research into the oncology space, I’ve also spoken with Hil Moss, co-founder and CEO of OncoveryCare, which provides an integrated survivorship care model. She underscored the importance of addressing the “survivorship gap” and equipping a new workforce to address their needs. This is critical because oncologists are already managing growing demand and most primary care physicians were not trained in cancer survivorship.
So where do we go from here? We need to aim for thorough and complete solutions that get at the real pain points.
By focusing innovation efforts in these areas, we can drastically improve the cancer care journey. Improving early detection will help to accurately identify at-risk patients and navigate patients to screenings and/or diagnostics, all while keeping both the patient and their care team informed. Improving clinical decision support tools will help capture critical data inputs and provide a complete and insightful output within the clinical workflow to augment the expertise of providers. Patients will be fully heard, seen, and supported while on treatment, and cancer survivors will receive patient-centric and comprehensive care for their unique needs.
All in all, this will ensure that patients who have received some of the worst news of their life get the best care journey possible.
If you are innovating in this space, or you’d like to discuss this topic with us further, we’d love to talk to you. Please email Keith Figlioli ([email protected]) or Yoola Adeniji ([email protected]).
